By Josh Bloom and Henry Miller
The development of new drugs is among the riskiest of business ventures. It now takes 10-15 years for a pharmaceutical company to get a new drug approved, and on average the cost exceeds $2.5 billion. To establish its safety and effectiveness, a candidate drug or vaccine undergoes a lengthy process of laboratory, animal and clinical studies, and then regulatory review is conducted by the highly risk-averse FDA.
The odds of success are not good. Only about 1/1000th of the candidate drugs screened even get into clinical trials, and of those that do, only about 20% are eventually approved for marketing. Even the rare success–a drug that is shown to be safe and effective and is approved by the FDA for marketing–is often a Pyrrhic victory: Only 20 percent of approved drugs will recoup more than their development costs.
The decades-long quest for treatments for hepatitis C, one of the scourges of the planet, offers an excellent example of some of the myriad, unobvious, possible pitfalls. In 1989, a new viral pathogen that caused infection of the liver was identified. Initially called “non-A, non-B” hepatitis virus and later renamed hepatitis C virus (HCV), it soon became clear that infection was very prevalent.
HCV currently infects approximately 3.2 million people in the United States and more than 170 million worldwide. About 75%–85% of people who become infected with hepatitis C virus develop chronic infection which can ultimately cause liver failure requiring a liver transplant, or cancer.
Treatments for HCV quickly became a major focus of research efforts in many pharmaceutical companies, both large and small. The resources committed to find treatments for this infection were enormous, but the science was especially difficult in spite of the fact that there was already a road map to follow. Much HCV research was modeled after the HIV cocktail approach—a combination of drugs, each of which acted via a different mechanism and possessed potent antiviral properties. In HIV/AIDS, this approach reduced the amount of circulating virus to levels so low that they could not be detected, a previously-inconceivable goal. Those drug cocktails transformed HIV infection from a certain death sentence to a manageable chronic disease.
HCV was a tougher nut to crack. After a decade of research and innumerable drug candidate failures because of toxicity or lack of efficacy, in 2004 scientists at Boehringer Ingelheim in Quebec hit the jackpot—or so it seemed–with a drug called ciluprevir. It virtually eliminated the virus in the blood after a few doses.
But a drug’s efficacy is only half the battle: Unexpected cardiac toxicity ended the hopes for ciluprevir. The effort did, however, provide an important proof of concept: that a specific antiviral drug could virtually eliminate HCV from the blood of infected patients.
In spite of the precedent and the application of prodigious money and manpower, it was not until 2011 that the first two specific antiviral HCV treatments—Victrelis (Schering Plough) and Incivek (Vertex)—were approved within a two-week period. One might think that this would have provided a bonanza to Vertex and Schering-Plough (now Merck) because their drugs, when added to the standard of care—an interferon plus ribavirin—roughly doubled the cure rate of that from interferon and ribavirin alone, which was in the 40-50 percent range.
But in spite of efficacy and relative safety of the drugs, it was not to be.
Incivek came roaring out of the gate, achieving sales of $1 billion within about six months of its release—among the best drug launches in history—but the bonanza did not last long. What happened was both fascinating and, under the circumstances, perhaps predictable.
In addition to eradicating the virus, another important objective of any new drug regimen for HCV was to eliminate the need for interferon because its side effects are awful and virtually universal: flu-like symptoms, depression, headache, nausea, vomiting, and joint pain, among others. To make matters worse, the recommended course of interferon plus ribavirin varied from six to twelve months, causing many patients to discontinue treatment because they could not tolerate the interferon.
Because both Victrelis and Incivek act through the same mechanism—inhibition of the protease enzyme that is required for viral replication—they could not be combined and used as a cocktail as was done in the case of AIDS. Therefore, one or the other had to be administered in addition to interferon and ribavirin—not in place of them. The holy grail of HCV research continued to be an interferon-free cocktail with a high cure rate. Unfortunately for Vertex (but fortunately for patients), it wasn’t far away.
The efforts of other companies working in this area (especially AbbVie, Gilead, Johnson and Johnson, and Bristol-Myers Squibb), although a bit behind Vertex, were beginning to pay off. The clinical results of their drugs were astounding, with cure rates approaching 100 percent. And in addition to the impressive efficacy of these newer drugs, they were effective without interferon.
This epic quest for ever safer, more effective and better tolerated treatments for HCV reflects the findings of a 2011 article in the journal Nature Reviews Drug Discovery, in which Joseph DiMasi and Laura Faden of the Tufts Center for the Study of Drug Development persuasively debunked the myth that drug companies purposely produce duplicative me-too drugs. They closely examined drug-development patterns and timing and found that the process is best viewed as “a race in which several firms pursue investigational drugs with similar chemical structures or with the same mechanism of action before any drug in the class obtains regulatory marketing approval.”
In other words, companies are not starting out to develop a me-too product any more than a marathon runner starts a race intending to be an also-ran.
There’s more to the HCV story. After seeing results of the pre-approval clinical trials of these newer drugs, many doctors began to advise their patients to delay treatment until some of the next generation of treatments were approved. This had a profound impact on Vertex: Sales of Incivek plummeted, and the company, which stopped selling Incivek in October 2014, announced a staff reduction of 370 employees—15 percent of its workforce. In addition, sales of Merck’s Victrelis, never that impressive to begin with, have fallen off the charts. The drug will never earn enough to recoup Merck’s development costs.
The final straw for Incivek was the approval of Gilead Biosciences’ Sovaldi (sofosbuvir)—an inhibitor of the viral polymerase called NS5B—which was the first HCV drug that could be administered without interferon. Sovaldi plus ribavirin provided cure rates of around 90 percent. In 2014, 24 years after the discovery of HCV, the holy grail of hepatitis C therapy had finally arrived.
At $1,000 per pill Sovaldi stirred up considerable controversy, but a full 12 week course ($84,000) isn’t much more expensive than interferon/ribavirin therapy, and is roughly 15 percent of the cost of a liver transplant, the only remaining option following liver failure.
Ironically, Gilead—the producer of Sovaldi, the first holy grail–took a big hit when AbbVie reached an agreement with Express Scripts, the nation’s largest pharmacy benefits manager, to exclusively sell Viekira Pak—AbbVie’s four-drug combination, which is about as effective as Sovaldi. But Gilead struck back by making its own deal with pharmacy giant CVS.
With other drug approvals looming, this jockeying will continue. Who benefits? Patients–who will have better medicines at lower prices because of the fierce competition among companies. This saga perfectly illustrates two points:
- Even when a drug goes through the 10+-year approval process, is found to be safe and effective and receives regulatory approval, for a number of reasons the company may not benefit financially.
- Second- and third-generation versions of the first approved drug often offer enormous advantages. This became obvious during the intensive efforts to find treatments for HIV/AIDS during the 1990’s, when drug companies were trying to improve upon the properties of Roche’s Invirase, the first HIV protease inhibitor.
Although first in class, Invirase had two major problems—bioavailability and gastrointestinal side effects. In subsequent years, nine other protease inhibitors were developed which were more potent, less toxic, and more bioavailable. These drugs formed the basis of the first drug cocktails, and their importance is reflected by the steep decline in the AIDS death rate in the U.S. beginning in 1995.
Nevertheless, skeptics continue to question the need for many new second- or third-in-class drugs and criticize the companies that develop them. Dr. Marcia Angell, the former editor of the New England Journal of Medicine, has complained for years that most new drugs are only minor variations of old ones–”me-too” drugs, which she has said are “unlikely to be better than existing ones for the same condition.” Drs. Donald Light and Joel Lexchin wrote in 2012 about an “innovation crisis” brought on because “pharmaceutical research and development turns out mostly minor variations on existing drugs.” And Rosanne Spector, the editor of Stanford Medicine, similarly charged that pharmaceutical companies “chemically rejigger an oldie but goodie, craft a new name, mount a massive advertising campaign and sell the retread as the latest innovative breakthrough.”
As illustrated by the rocky path to successful, financially rewarding treatments of HIV/AIDS and HCV, their view of the landscape is overly simplistic and, in the final analysis, dead wrong.
“Me, too” drugs are valuable in several respects. Patients experience different side effects from different statins, for example, making the availability of multiple choices not only beneficial, but also life-saving. And even if two drugs are each effective in 40% of patients with a particular symptom or disease, each of them may not work in the same 40%. If the drugs are effective in different populations, the unavailability of the second drug could deprive a large number of patients of the medicine they really need. Practicing physicians know that for certain conditions—such as treating pain, psychiatric disease or the symptoms of multiple sclerosis—patients whose conditions seem indistinguishable from one another sometimes do better on different drugs.
Having alternatives—”me-too drugs”—available is in the best interests of patients, as illustrated by the hepatitis C saga, which shows how the research efforts of the pharmaceutical industry can result in cures for a public health scourge that was once poorly treatable. In the end, the development of a cascade of “me, too” drugs benefited individual patients and society. That’s the bottom line.
Josh Bloom, Ph.D., is a medicinal chemist and the Director of Chemical and Pharmaceutical Sciences at the American Council on Science and Health. Henry I. Miller, M.D., a physician and molecular biologist, is the Robert Wesson Fellow in Scientific Philosophy and Public Policy at Stanford University’s Hoover Institution and a fellow at the Competitive Enterprise Institute. He was the founding director of the FDA’s Office of Biotechnology.
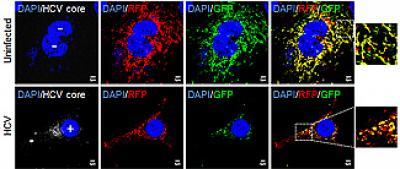
Self-destructing hepatitis C-infected cells image credit: UC San Diego School of Medicine.
This article first appeared in Forbes in slightly modified form. Republished with permission.



Comments